Syndromic surveillance is a public health campaign that can track symptoms of disease in the community and use the resulting insights to predict hospital utilization during a surge, inform reopening, enable quick policy changes, or reallocate resources. COVID-19 is a clear candidate for this kind of aggressive monitoring. Here are some examples why:
- Weeks after noticing low infection rates, which led them to relax restrictions on distancing, several U.S. states suffered their worst outbreaks. Had they been able to analyze the trajectory of COVID-like symptoms, they might have learned that they were on the verge of a breakout and the have taken action to reverse the relaxation of restrictions, as well as use predictive modeling to predict which hospitals would see patient spikes.
- Spikes in COVID-19 admissions have left many hospitals without enough remdesivir, which can shorten recovery times and perhaps reduce deaths from the virus. Accurate predictions of spikes could allow hospitals with surplusses of remdesivir to transfer it to the places where it will be needed.
- COVID-19 testing is nearly impossible to get in many areas that are centers of infection. Better predictions could have spurred these states and municipalities to set up more test centers.
Premier Inc., a health IT firm that employs data and machine learning to solve a variety of health care industry problems, is using it to modernize syndromic surveillance. They call on states to work with their local providers in using the system to monitor COVID-19 symptoms in real time. Based on machine learning, the system should work much faster and produce more accurate predictions.
Because the Premier system is new, we don’t have on-the-ground results to confirm these hopes. But I am publishing this article to prompt states and providers to take a close look at the solution.
A Serendipitous Initiative
I talked this past Monday with Mike Alkire, President of Premier, and Ryan Nellis, the Chief Commercial Operations Officer of Stanson Health, a Premier Company. They told me that they got the COVID-19 system working by repurposing a system already embedded for a very different use in several big electronic health record systems.
As background, Premier offers predictive analytics and clinical decision support quickly, sometimes in real time, to hospitals and ambulatory physicians. This can serve various needs ranging from clinical interventions to improving supply chains. To derive the insights, Premier integrates its analytics into all the most popular U.S. patient EHRs, including Epic, Cerner, and Athenahealth. Over 4,000 hospitals and 175,000 other provider organizations tap into Premier’s analytics today, a network that can be useful to scale up COVID-19 surveillance fast.
The system they developed was designed to help hospitals comply with imaging regulations designed by the Centers for Medicare & Medicaid Services, as part of implementing the Protecting Access to Medicare Act of 2014 (PAMA). In brief, radiologists and imaging centers are penalized for prescribing unnecessary CT scans or other expensive imaging tests without first consulting a qualified clinical decision support technology. It’s extremely valuable to a health care provider to gather all the data relevant to this decision in real time for each patient before prescribing the test. Premier’s Stanson Health designed a system to get the data on which they could provide clinical decision support and analytics to guide decisions.
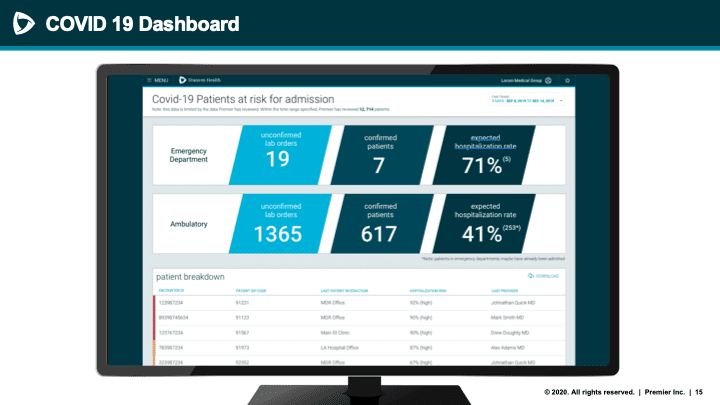
After the onslaught of COVID-19, Premier realized they could repurpose this system to track symptoms in an ambulatory population in real time. They wanted not only to identify who had COVID-19 symptoms, but to determine which patients are likely to require an upcoming hospitalization before the actual admission occurs. This called for intensive analysis of patient data: age, vitals, gender, comorbidities, and more.
They based their initial model on data published by a hospital in the COVID-19 hot spot New York City, describing all the data the hospital collected on its patients and what the data told them about the likely trajectory of the patient.
Premier could get all the data they needed from the health records, both in-person visits and telehealth. But interpreting it programmatically wasn’t always easy. Sometimes, key diagnostic criteria are buried in unstructured text notes, and doctors may use a lot of different words or abbreviations for essential symptoms such as “shortness of breath”. Premier used natural language processing (NLP) to extract the necessary data from the text.
Uses for Syndromic Surveillance
We will learn over the next six weeks how well Premier’s syndromic surveillance does its job, and whether states, cities, and health care institutions can benefit. We know that our current surveillance efforts are not working well. Tests are not widely enough available, take too long to report results, and provide too many false negatives. It seems time for a more high-tech approach.
Some potential uses for Premier’s data are:
- Instead of shutting down a whole state during an outbreak, authorities can place restrictions on particular ZIP codes where they expect the outbreak to get worse.
- A hospital can convert part of its facility to an ICU of COVID-19 specific ward, if predictions indicate an upcoming spike.
- A hospital can order more PPE, drugs, and other equipment to prepare for the spike.
- Clinicians can better determine the risk that a particular patient will need hospitalization or the ICU, and watch at-risk patients closely.
But Premier is asking clinical settings not to wait six weeks or more for initial results. Lives may be saved if large swaths of the country try their solution.
This article is part of the #HealthIT100in100
Listen and subscribe to the Healthcare IT Today Interviews Podcast to hear all the latest insights from experts in healthcare IT.
And for an exclusive look at our top stories, subscribe to our newsletter.
Tell us what you think. Contact us here or on Twitter at @hcitoday. And if you’re interested in advertising with us, check out our various advertising packages and request our media Kit.













