In theory, we all love the move to value based care. Why aren’t we paying healthcare providers to improve care. It just makes sense. In fact, the fee for service model in many ways feels so unnatural. While the theoretical value based care sounds good, getting there is much easier said than done. Translating the simple idea of value based care into regulations and reimbursement is a really hard thing to do.
I’ve often asked the question, “Is value based care just a regulation and reimbursement hoop jumping activity?” Does he who can jump through the hoops the best win? Or is it really the person who improves the care the most win?
I found two Twitter threads discussing ACOs that may shed some insight into not only ACOs, but the shift to value based reimbursement. Plus, I think it might help to answer the question above.
The first ACO thread is in response to an NGACO report from CMS that was shared by David Muhlestein.
Tagging some of my ACO friends: @ThomasPMerrill @KatedeLisle @The_ACLC @Farzad_MD @Travis_Broome @WillBleser @valeriealewis @Michael_Chernew @CHColla @LeavittPartners @nick_c_bluhm @TimGDC https://t.co/zdVU6zztAY
— David Muhlestein (@DavidMuhlestein) August 28, 2018
In response to David’s tweet, Adam Solomon offered his perspectives in this tweet storm:
Sorry to chime in late. Our NGACO experience was very interesting. Our benchmark was based on our historical utilization for a similarly attributed population. They then added a very low trend factor to come up with a final target.
In the end, our PBPM cost was actually lower than the benchmark, but we still owed over $5 million to CMS. What happened?
Because the baseline year risk was calculated in the 2014 model and year 1 was the 2016 model, they couldn’t directly compare the acuity of the two populations. Therefore, the utilized a ratio comparing our trend to that of others. Our RAF score didn’t jump as much as theirs.
So our RAF “decreased” suggesting our active population was healthier than our baseline. That accounted for over $2.5 million dollars of “loss.”
The other hit was the way they calculated stop loss. Sure, there was an elective level of aggregate stop loss, but they also assigned a PBPM cost for individual stop loss based on expectations for number of patients with claims over the 90th percentile.
Because California has historically high costs, they estimated that we would have an abnormally high number of patients that exceeded that threshold. That was something like a $20 PBPM hit or another $3.5 million of artificial cost to us.
In the end, although we saved CMS money, we still needed to pay them for our “loss.”
Separate from that, the NORC Report noted above uses a different methodology to estimate savings. Instead of using ourselves as a baseline, they used a regional reference population.
The saddest part for us was that our utilization was always at the top end with little room for improvement. As an example, here’s admits/k for year 2 NGACOs. We’re dark blue.
In a separate tweet storm, Farzad Mostashari, Former National Coordinator at ONC and now Founder of Aledade offered this look at the ACO results:
1/ 2017 #MSSP #ACO Results!
ACOs have scaled rapidly across the country!In aggregate, the 472 ACOs were accountable for nearly 9 million Medicare beneficiaries and $95 Billion- that’s a quarter of all fee for service, and almost half of the entire Medicare Advantage market.
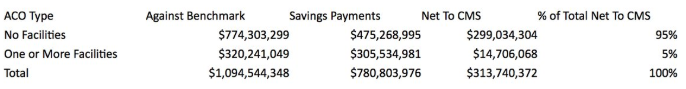
2/ If you add up all the actual costs versus benchmarks, these 472 ACOs were collectively $1.1B under their benchmarks (more on whether that’s the right counterfactual later).
Medicare shared $780 million in payments with the ACOs, netting the taxpayer $313M
But wait!There’s lots of evidence that the benchmark under-estimates the savings produced. @JMichaelMcW et al have shown convincingly that a true “difference in difference” approach would show substantially higher net impact.
The green eyeshades folks at CMS OACT said add 60%
3/ So that means that the best guess for MSSP savings is actually $1.75B in 2017, with Medicare paying out $780M (45%)- not a bad deal for the taxpayer!!!That does NOT count savings that come from lower costs to the taxpayer from Medicare Advantage rates that are keyed off FFS
4/ Here’s how the CMS actuaries put it:
And on quality- the average ACO earned 92% on their quality scores- and the scores improve the longer you are in the program according to the ACO Rule’s Regulatory Impact Assesment.(The Aledade average quality score applied was over 95%, and as high as 99.8% #GoKANSAS)
6/ Lemme say that again….ACOs saved Medicare over a Billion dollars in 2017.
Cheaper than FFS, cheaper than MA.
And they did it without cutting payments to doctors or narrow networks
And they did it with higher patient quality.
That’s called delivering what was promised
7/ the Track 1 ACOs more than held their own here
Best guess is that Track 2/3 generated 190M in savings (w 60% spillover) and received $95M (50%)
Track 1: $1.5B in savings, $685M in payments (44%)
(I’m still a believer in moving to 2-sided risk to help weed out ACO squatting)
8/ You know what was a great investment? Giving small and rural physician-led ACOs an advance payment to help them invest in infrastructure and setup costs.
It was critical to the success of several of our @AledadeACO
More commercial payors should do this!
9/ But what this initial release does not help us do is see which type of ACOs are creating the most value.My guess is that it’s not much different from what the CMS actuaries found for PY 2016- ACOs that include hospitals and directly control more of the cost of care do worse
10/ The “low revenue” ACOs (in the OACT analysis – less than 10% of total cost of care came to them) were only a third of the lives in the program, but generated roughly 98% of the savings.THAT is why in the ACO Rule CMS proposed letting them stay in low risk models longer
11/ That was the entire thesis behind “the paradox of primary care leadership” that informed the founding of @AledadeACOThat is also why @AledadeACO partners with independent physician practices, not hospitals like others do.
Health Reform and Physician-Led Accountable Care
Even though most adult primary care physicians may not realize it, they each can be seen as a chief executive officer (CEO) in charge of approximately $10 million of annual revenue. Consider that a t…
https://jamanetwork.com/journals/jama/fullarticle/186135912/ A quick analysis by the amazing @Travis_Broome divides these 2017 results by whether the ACOs included a “facility/CCN” (CAH, RHC, FQHC don’t count for this purpose) –
Same pattern- 95% of the savings are coming from the ACOs that don’t include hospitals.
13/ Only 3.5M of the 9M ACO-attributed benes were cared for by the smaller ACOs that didn’t include a hospital facility- and they generated 95% of the savings.If you’re an independent practice seeing these results and the policy direction, why would you join a hospital ACO?
So how did @AledadeACO do?We are always very transparent with our results- even when things didn’t go our way- to look for ways to be better, and to make policies better that are holding back broader success.
This article 2 years ago was full of pain.
The Opportunities and Challenges of the MSSP ACO Program: A Report From the Field
This article provides a detailed description of a Medicare Shared Savings Program accountable care organization (ACO)’s actions and results, to increase understanding of the challenges and opportunit…
https://www.ajmc.com/journals/issue/2016/2016-vol22-n9/the-opportunities-and-challenges-of-the-mssp-aco-program-a-report-from-the-field15/ This was a good year for @AledadeACO
Only 1/7 freshmen ACOs made savings- but we have learned to set expectations- it’s a long game.
But 5/8 ACOs that were sophomores or older will get checks.
And 2/3 that didn’t get MSSP crushed it in commercial contracts.
16/ But I’m more proud that EVERY ONE of our @AledadeACO have measurably improved health for the patients we are accountable for.
We have increased wellness visits, transitional care, and chronic care management- and that’s translated into lower ED visits and readmissions
17/ So where do we go from here?The #MSSP #ACO program has been a hugely successful motivator of nationwide transformation, but it can be reformed, and I believe @SeemaCMS is on the right track.
Here’s what I would expect might change between the NPRM and the final ACO rule:
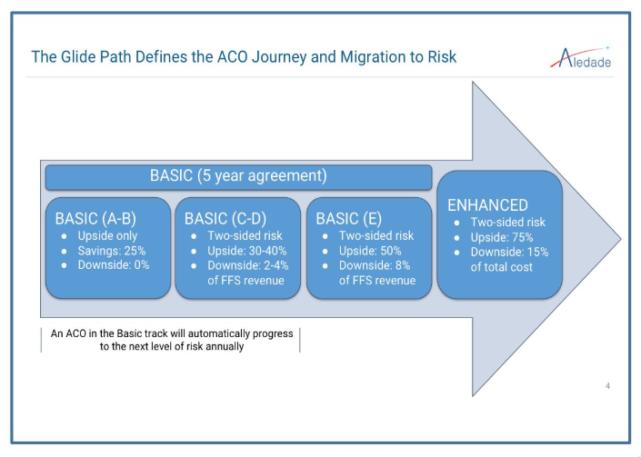
18/ The GlidePath to risk reduces ACO squatting, and brings revenue-based downside risk to MSSP, but the lowered gainshare in 1st 2 years (25%) is not enough to get new entrants and ACO investments.
(as suggested) “low revenue” ACOs should get higher gain-share and lower MSR
19/ The refined benchmarking method gives greater predictability by allowing risk adjustment and regional trending-which is great!
But the cap on risk adj (3% over 5 years?!) don’t control for rising risk and introduces gaming on falling riskInstead of a cap, do renormalization
20/ Concern about “windfall profits” led to an ill-advised proposal to cap regional efficiency at 5% – In Medicare Advantage if you are efficient, you get to keep the difference, which has spurred huge innovation in the space. why blunt improvement? 100% tax brackets are not good
21/ Credit to CMS for trying to fix the unintended “regional comparator” problem- where rural ACO savings are reduced in direct proportion to market share. But the “national trend blend” proposal makes NO SENSE.
Let’s just take ACO benes out of the regional comparison please!
22/ But the biggest impact of these results on the proposed rule should be on the idea that the way to benefit the Trust Fund is to protect it from ACO earnings.
These caps, etc reduce ACO earnings- and ACO motivation/participation- and therefore reduced benefit to Medicare
23/ The NPRM RIA estimates through 2024 these caps push $390M in lower ACO earnings, but lower ACO participation under these policies will INCREASE claims costs by $60M- and would prevent beneficiaries from receiving the benefits of the program. That’s not the right balance
24/ The magic of accountable care is when physicians & Medicare partner together to sustainably align financial incentives, help beneficiaries and the Trust Fund.Medicare hasn’t behaved like some commercial payers who are still seeing zero sum. Let’s hold onto that partnership
I’ll let you be the judge after reading through these threads. Are ACOs going to really improve healthcare and lower costs? Will the best healthcare win? Or will the people who understand the government rule making process and healthcare accounting be the big winners?
As I read through these, it seems like you better get your accountants and healthcare policy experts ready. That brings joy to every doctor’s ears…I’m sure!